We had an interesting consult a few weeks ago.
The patient was an elderly gentleman who recently underwent an EGD for gastritis-like symptoms. A few days after the procedure he received a call from his gastroenterologist telling him that he had H.
Pylori and needed to start an antibiotic. He was prescribed PrevPac for 10 days. He almost immediately began to feel worse. His wife ultimately stopped giving him the PrevPack after about four days of increasing weakness, lethergy and nausea. Despite stopping the new medicine the patient continued to deteriorate. He was admitted about 2 weeks after the EGD.
His creatinine had risen from a baseline of 1.2 mg/dL to 4.5 mg/dL. Our initial thought was that he was pre-renal. We prescribed 0.9% saline but the patient didn't respond, and his creatine continued to rise.
One clinical pearl that I repeatedly teach fellows is not to under treat pre-renal azotemia. If you think the patient is volume depleted give enough fluid that the next day if the creatinine has not improved you will be convinced that the patient is no longer volume depleted. You want to fully rule-out volume depletion after the first day.
This patient didn't respond to fluids so we reevaluated the history. PrevPac, what's in that?
- Lansoprazole
- Amoxicillin
- Clarithromycin
Clarithromycin is a potent inhibitor of CYP3A4 so it interacts with a lot of medications. Our patient was on simvastatin. Let's check out what does Dr. Google has to say about that:
We check his CPK and its 8,000 almost a week after he stopped taking the Clarithro.
Rhabdo induced acute kidney injury due to a drug interaction.
Rhabdomyolysis secondary to a drug interaction between simvastatin and clarithromycin. Clarithromycin is a potent inhibitor of CYP3A4, the major enzyme responsible for simvastatin metabolism.
Effects of Clarithromycin on the Pharmacokinetics of Simvastatin. Compared with simvastatin alone, coadministration of clarythromycin and simvastatin significantly increased the peak concentration and the area under the curve for simvastatin by approximately 8-fold (p<0.0001). Levels of simvastatin acid were also significantly (about 14-fold) higher during clarythromycin treatment compared with simvastatin alone (p<0.0001).
If the figures on pharmacokinetics from that last article are to be believed then 500 mg of clarithromycin magnifies 80 mg of daily simvastatin to an equivalent daily dose of 640 to 1,120 mg.
Rhabdomyolysis induces acute kidney injury from myoglobin. Myoglobin can precipitate in the presence of acidic urine. The heme component of myoglobin can generate free-radicals which can damage lipid membranes. Patients develop vasoconstriction in response to rhabdomyolysis, both from the direct effect of the myoglobin on the renal vasculature and due to the movement of intravascular fluid into the damaged muscles. This gives a pre-renal picture on the fractional excretion of sodium.
Evaluating volume status can be tricky because patients will often have peripheral edema from the inflammation associated with the rhabdomyolysis. Additionally the BUN:Cr will often be low as the creatinine tends to rise quicker in rhabdomyolysis than in other forms of renal failure. This is usually explained by the release of intramuscular creatinine rather than just a failure to clear creatinine. The younger age and increased frequency of men suffering from rhabdomyolysis may also play a role in this observation.
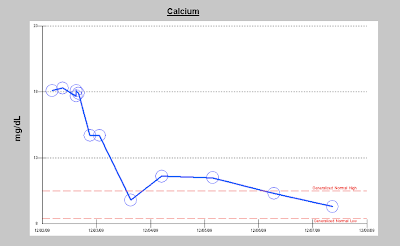
The electrolyte abnormalities of rhabdomyolysis:
- Hyperkalemia
- Hyperphosphatemia
- Hypocalcemia (early)
- Hypercalcemia (late)
- Hyperuricemia
- Anion gap metabolic acidosis
The NEJM recently did a nice
review of rhabdomyolysis which presents the recent inconclusive data on alkalinization (not proven to be helpful but the animal/disease models make it look like the right thing to do), mannitol and diuretics and use of high flux dialyzers.
The Annals of Internal Medicine recently published a
review of Statin-Related Myopathy. Here is what they had to say about drug interactions:
Because simvastatin, lovastatin, and atorvastatin are primarily metabolized through the cytochrome P450 3A4 (CYP3A4) isoenzyme (43), inhibitors of CYP3A4 could theoretically increase serum statin levels and exposure to susceptible tissues. Drugs known to interact with statins include protease inhibitors, cyclosporine, amiodarone, and fibrates (44, 45). Protease inhibitors are potent CYP3A4 inhibitors and thus can increase up to 30 times the plasma concentrations of certain statins (45, 46). Consequently, both simvastatin and lovastatin should be avoided in pa- tients receiving protease inhibitors (42, 45, 47). Cyclosporine is a potent inhibitor of not only CYP3A4 but also several membrane transporters, and it increases the phar- macokinetic area under the curve of statins by 2- to 25- fold, with many reported cases of rhabdomyolysis (44). Statin dosages in patients receiving cyclosporine have therefore been limited to 5 mg/d for rosuvastatin, 10 mg/d for simvastatin and atorvastatin, and 20 mg/d for lovastatin (42, 47–49).
Pravastatin is not metabolized by the P450 system but is excreted renaly. Fluvastatin and rosuvastatin are metabolized by an alternative enzyme, CYP2C9.


















 :
: