SPRINT. We talked about the impressive results but really focused on the very selective patients population and how it was not consistent with a lot of patients we see in clinic. We also focused on how they assessed blood pressure and how different it is than standard blood pressure assessment.
The next study was HOPE-3 shows that when you apply what you know from SPRINT but use a standard blood pressure assessment and pair it to a less sick population you get a negative result.
Then we looked at PATHWAY-2 to put add some evidence to the question of how should we treat resistant hypertension.
Then we finished with "Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials" a fascinating meta-analysis that looked at dose response curves, and side effects. Really interesting paper. H/T Ricky Turgeon PharmD. The conclusion from the data is that adding additional drug classes at lower than standard doses results in a nice blood pressure improvement with a clean side effect profile.
Other suggestions that didn't make the 40 minute cut:
@kidney_boy HYVET— Ross Nesbit (@RossNesbit) December 30, 2016
Treatment of Hypertension in Patients 80 Years of Age or Older
Agree this is an important study.
Agree this is an important study.
@kidney_boy Bit late to this but ASCOT-BPLA— Annette Neary (@feline_charm) December 30, 2016
Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial
@kidney_boy ACCORD BP (lower not always better, esp. In Diabetics) since SPRINT included non-Diabetics. Would also include HYVET— James Pritsiolas, MD (@Nephro_Doc) December 29, 2016
Effects of Intensive Blood-Pressure Control in Type 2 Diabetes Mellitus
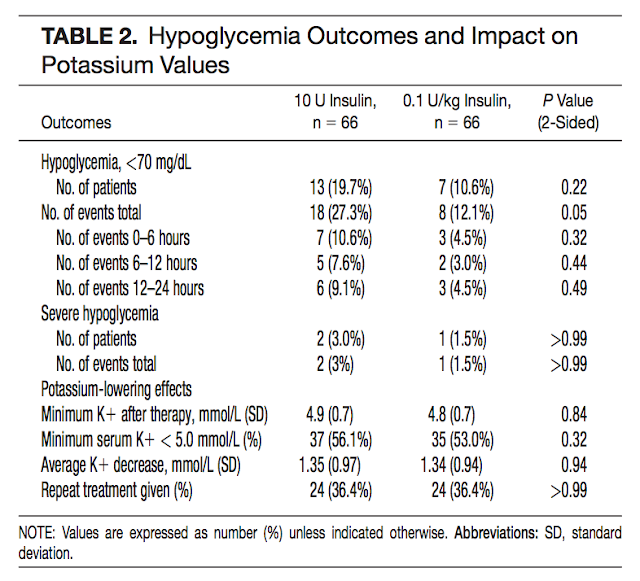
This is the opposite side of the SPRNT coin. Low blood pressure appeared to be of no benefit and possibly harmful (Table 2). Nice reduction in stroke though (Figure 2).
@kidney_boy ... and Symplicity HTN-3— Indranil Dasgupta (@idasgupta7) December 29, 2016
A Controlled Trial of Renal Denervation for Resistant Hypertension
The mother of all medical reversals. Great study. Totally upset a runaway freight train of interventions. To me this shows that industry sponsored trials (when designed with the intension of FDA approval) are not marketing shams but can add clarity to medical knowledge.
The mother of all medical reversals. Great study. Totally upset a runaway freight train of interventions. To me this shows that industry sponsored trials (when designed with the intension of FDA approval) are not marketing shams but can add clarity to medical knowledge.