Makoto Kuro
Emerging role of Klotho
Klotho mouse has accelerated aging
due to insertion of gene missiong gene X by accident.
first model of human aging with multiple phenotypes.Question what is gene X
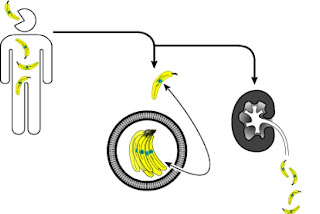
single pass transmembrain protein
it has some siaqlidase activity
gene expressed predominant\ly in the kidney and a little in the brain
does over expression of klotho surpress aging?
over expression extends mouse life by 30%
expressed in the distal convoluted tubules with weak expression in PT
the extracellular domain is clipped by ADAM 10 and then is a soluble factor
klotho -/- has similar phenotypes as FGF23 -/-
FGF is phophaturic hormone from the bones
gain of function causes hypophosphatemic rickets (vit D resistant)
FGF23 binds to FGF23 receptor plus Klotho
FGF23 requires klotho to activate FGF signaling
FGF lowers 1-alpha hydroxylase and increases 24-hydroxylase (deacticvate 1,25)
`
FGF?Klotho system surpresses PTH
agiing like phenotypes are caused by phosphate toxicity
soluble/secreted klotho independent of FGF23 increases renal phosphate wasting
sialidase activity activates TRPV5 which increases Ca current.
Link between |Klotho and CKD.
Mice lacking Klotho and ESRD share: casc calcification and hyperphosphatemia
mice with over expression of klotho are more resistant to vasc calcification and hyperphosphatemia in CKD model.