Pretty stunning. He's young and, despite some tobacco and a generous BMI, he seems healthy. He eats whole foods and is physically active. He does not have diabetes or hypertension.
Last night he was asking about whether a stress test could have made a difference. Two years prior, he experienced symptoms consistent with atypical angina. He had two episodes of chest pain, both associated with activity, but not regularly reproducible. My friend discussed these symptoms with a doctor who did an initial work-up to get a Framingham risk score but my friend never followed up. So the question my friend had was simply, "Should an exercise-stress test have been done on my initial presentation?"
So let's look at the data. During the hospitalization a lipid panel was done which allows us to calculate his
Framingham Risk:
Fifteen percent, intermediate risk. Last year the NEJM
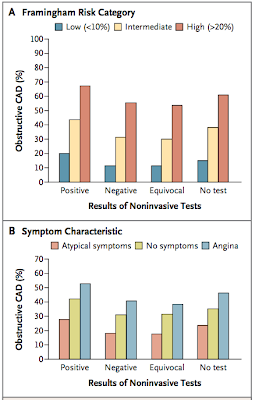
published a great article (at least by my pee-stained eyes) that looked at the diagnostic yield of cardiac catheterization and non-invasive testing. The data is not very encouraging. Here are the key figures, at least for my question:
The top panel looks at the diagnostic yield of noninvasive heart tests, and stratifies patients based Framingham risk scores. What should be obvious is that the there is much greater differentiation of outcome within series (same stress test result but varying Framingham scores) than compared to fixed risk scores and varying non-invasive test results (i.e. the red arrow is more important than the bue one):
That means that, had my friend gone for a stress test, the likelihood of having a positive cath would have gone from 35% with a negative test to 42% with a positive stress test. It's hard to imagine that a rational medical plan would change with that additional data. Stated another way, would any doctor recommend a cardiac cath with a pretest probability of 42% but not order that same test with a pre-test probability of 35%? Doubtful.
The other thing which is notable, in panel B is that atypical angina is protective compared to no symptoms at all. My friends symptoms were definitely atypical. Here are the definitions according to
UpToDate:
- Definite or classic angina — Substernal chest discomfort characterized by all of the following characteristics: a typical quality and duration, provocation by exertion or emotional stress, and relief by rest or nitroglycerin
- Probable or atypical angina — Chest pain with two of the three above characteristics
- Nonanginal or nonischemic chest pain — Chest pain with one or none of the above characteristics
So it looks like my friend's primary care doctor was using evidence based medicine. He did not rush to a stress test or other noninvasive test because the Framingham Risk Score was a better predictor of cardiac disease and my friend's description of the chest pain, oddly, put him at a lower risk of coronary disease than no symptoms at all.