Okay nephrologists, we have suffered the slings and arrows of outrageous trial after trial going
against us. It is time to put down those depressing journals full of non-significant P values and stretch our imagination. It is time to design our own dream randomized controlled trial. The assignment is to target the most important question you see in nephrology today and design a trial to answer it. One question not enough for you? Design a trial to answer two questions ACCORD style, two questions not enough, go all AASK and design a 2x3 factorial design. Money no object, forget about pesky IRBs, let your mind free and create the trial which will meaningfully push back the walls of knowledge.
After you post your entry at your site of choice,
UKidney will host a summary with a link for each entry and gather votes for the best. You can take a look at Jordan Weinstein's Dream RCT
here.
And may the IRB be ever in your favor.
My Dream RCT: Background
Humans have higher uric acid levels than almost other animals. This is primarily due to the lack of uricase, but also due to our efficient renal reabsorption of filtered uric acid by URAT1 and GLUT9. Traditionally, it has been believed that hyperuricemia causes renal disease by precipitating intraluminal crystals, analogous to gout crystals in the joints. More recent data however, implicates lower levels of uric acid in hypertension and chronic kidney disease through suppression of nitric oxide formation, stimulation of inflammation through NF-kappa beta and other mechanisms. Supporting these theories are animal studies that show febuxostat and allopurinol reduce renal damage in multiple models of kidney disease (
here and
here).
Epidemiologic studies linking uric acid to chronic kidney disease show a definite association but whether the uric acid causes the kidney disease is difficult to tease out. Attempts to show that have shown mixed results.
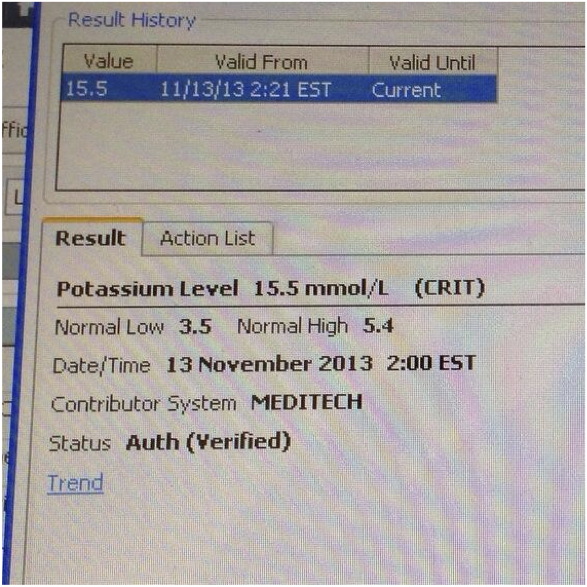
Four interventional studies have attempted to answer this question in humans:
- Siu et al. randomized 54 hyperuricemic patients to placebo or enough allopurinol to normalize the hyperuricemia. After a year there was less creatinine progression with the allopurinol.
- Goicoechea et al. randomized 113 hyperuricemic patients to no therapy or 100 mg of allopurinol for two years. They found improved renal function with drug compared to modest loss of function without allopurinol. And intriguingly they also found a significant reduction in cardiovascular events.
- Shi et al. evaluated 40 patients with IgA nephropathy for 6 months. This was a negative study with no effect on GFR (but that is hardly surprising given the very short follow-up time), but it did have a beneficial effect on hypertension
- Momeni et al. performed a 4 month double blind, placebo controlled trial of type 2 diabetics and found a reduction in proteinuria.
 |
| From Goicoechea's study of 100 patients |
More information can be found on uric acid in my
grand-rounds or in an excellent
Narrative Review from AJKD.
Despite multiple randomized trials showing allopurinol to be effective in CKD, don't be fooled, both trials were tiny with limited follow-up.
 |
| Diameter of the circle is proportional to the trial size |
Given that background, it seems well past time to commit to finding a definitive answer to the question of whether we should be using xanthine oxidase inhibitors to slow the progression of chronic kidneys disease.
Scouring
ClincalTrials.gov I could find only one study that is addressing this hole in our knowledge. The
Joslen Center is planning, but has not yet started enrolling, a double-blind, placebo controlled multi-center trial of allopurinol in type 1 diabetics. The study design looks pretty sharp with iothalamate GFRs after 3 yrs of therapy being the primary outcome. However I am dreaming bigger and want my study to apply to all patients, not just type 1 diabetics with nephropathy.
My Dream RCT: methods
My dream study is a placebo controlled, double-blind, multi-center, randomized controlled trial. The study population is CKD stage 3 patients with hyperuricemia (uric acid over 7 mg/dL). This represents a lot of the population with kidney disease which means that the results, if positive, would literally influence the treatment of millions of people. The study will use block randomization and quotas to assure a varied distribution of renal disease. At least a third of the population will have proteinuria and half will have diabetes.
All patients with proteinuria would need to be on RAAS inhibition unless they could not tolerate it. Blood pressure would be treated by the treating physician using JNC8 guidelines. Patients would be randomized to one of three arms:
- placebo
- allopurinol 100 mg daily
- fubuxostat 40 mg daily
If the uric acid remained above 7 after one month of treatment the study drug would be doubled. Patients intolerant to the assigned drug could cross over to the other study drug. Study coordinators would signal a central dispensary that patients were intolerant and the dispensary would change patients on placebo to another placebo (essentially no change at all) and patients on one of the xanthine oxidase inhibitors would cross over to the other xanthine oxidase inhibitor. By employing this three arm approach we will be able to assess if any affects is due to a specific xanthine oxidase inhibitor or a more general effect of lowering the uric acid. It will also allow us to get detailed data on the tolerability and safety of the drugs in CKD.
The primary end-point is a composite of doubling of serum creatinine, death or dialysis.
Secondary endpoints are achieved ambulatory blood pressures, hospitalizations, new cardiovascular events, and gout.
This study would have results applicable to the millions of people with chronic kidney disease and would open up the first novel front in the war on CKD since the wide use of RAAS inhibition.
UPDATE
Apparently this RCT is not a dream but a trial that is going to be done, from
Swapnil Hiremath:
Looking through the
registry data the
CKD-FIX trial sounds like a pretty close match to my Dream RCT, my one concern is they were supposed to begin enrolling patients in March of 2012 but have yet to enroll they''re first patient (according to the registry). Anyone know if this study is still going to happen?
UPDATE 2
It is on. CKD-FIX to start enrolling next month.