Monday, October 26, 2009
Acid-Base Chapters (Chapters 10-16) from Fluids
Chapter 10: Introduction to Acid-Base
Chapter 11: Introduction to Metabolic Acidosis
Chapter 12: Non-Anion Gap
Chapter 13: Anion Gap Metabolic Acidosis
Chapter 14: Metabolic Alkalosis
Chapter 15: Respiratory Acidosis
Chapter 16: Respiratory Alkalosis
Dysnatremia chapters (chapters 6-9) of Fluids
Chapters 6 and 7: Hyponatremia
Chapter 8: Hypernatremia
Chapter 9: Polyuria/Polydipsia
Why I love the Mac
To bring my readers the Fluids book I had to merge multiple PDFs into a single document. For example, the Hyponatremia chapter exists on my hard drive as 4 separate pagemaker files. These can be converted to four separate PDFs. To put them together is trivial in Mac OS X. No Acrobat Pro or other nonsence needed:
And from with a little more context from Mac OS X Hints
Use Preview to open up the two PDFs you would like to merge. Choose View » Show Sidebar (or click the Sidebar button). Make sure both PDFs are visible on the screen at the same time. When the Sidebar pops out, you will see a graphical representation of the pages in your PDF document. Simply drag the page, or pages (use Comand to select multiple pages) from the Sidebar of one PDF to the Sidebar of another. You have now merged pages from two separate PDF documents.
So easy. So simple. So elegant.
The first five chapters of the Fluids book
Chapter 1: Moles and Water
Chapter 2: Water, Where are You?
Chapter 3: Starling's Law
Friday, October 23, 2009
The Fluid and Electrolyte Companion has been locked up
The Fluid, Electrolyte and Acid Base Companion was a book I co-wrote during my residency. We started the book in 1995 after graduating and finished it during the summer of 1999. The book came out in January 2000.
The book was a home brew project with no professional assistance. We researched the book, wrote the text in Adobe Pagemaker and did the illustrations in Adobe Illustrator. All the computer work was done on Apple computers. This was a time before OS X and we suffered through the dark days of System 7.5.5, the Vista of Apple operating systems.

When the book went to press the source files were primarily a mixture of Pagemaker 6.5 and Illustrator 8.0. Significantly, we never upgraded to Pagemaker 7.0.

After we finished, Adobe put Pagemaker out to pasture and replaced it with InDesign. Adobe never released a version of Pagemaker that ran natively in OS X and the tools they created for moving from Pagemaker to Indesign required the files to be Pagemaker 7 files. Our 6.5 files were an evolutionary dead-end. No way to get them to Indesign. Then, as my interests turned away from the book and toward the rest of my life I started snipping the threads that allowed me digital access to the Fluids files. In 2001 I transitioned from OS9 to OS X and had to use Classic to open up the book or use Pagemaker. In 2008 all of the Macintosh's in my house (my laptop, desktop, and wife's laptop) were finally upgraded to Intel processors which meant that they could no longer run Classic which locked me out of the book. Functionally it was no different than if my hard drive had crashed and I had lost all of my back-ups.
When I started this blog, one of the things I thought I would use it for would be as a tracking tool as I rewrote and modernized the original Fluids book. Well for the last 18 months I have been stuck on the very first step of this process: getting electronic access. I finally solved that problem by getting my hands on a vintage 12 inch PowerBook that was in one my parent's closets.
Last week-end I found my old Pagemaker and Illustrator disks and installed them under classic. Then I looked deep in some old hard drive back-ups to find all of the fonts needed to render the files. Finally, after some deep Googling, I came across this work-around to create a PDF from Classic. So here is the first chapter of the Fluid, Electrolyte and Acid Base Companion:
I hope to follow this with an edited version of this chapter and then move on to the subsequent chapters and really provide a modern, comprehensive tutorial towards fluids and electrolytes aimed at medical students and residents.
David Pogue did a nice piece on this for Sunday Morning
In the future, I'm going to need to try this and see if it allows me to run my old programs on my current laptop.
Thursday, October 22, 2009
The things patients bring in
The other day one of my patients brought in a list of the 50 most prescribed medications according to the AARP. Jackpot.
I have transcribed the data into excel so I could abstract some of the data. The raw excel file is here.
I have three charts from the excel file that are interesting, the first is just a graph of the number of prescriptions with the retail cost overlaid. Can you spot the brand name drugs:
I then simplified the data by removing the noise from the individual drugs and used the indications for each drug. Here is that data by number of prescriptions and then by cost:
You can see the disruption caused by the brand name drugs which catapult PPI (ulcer/heart burn medications) from 5% of the prescriptions to 17% of the cost and take statins (cholesterol) from 9% of the prescriptions to 18% of the cost. Can you imagine how the chart looked before Zocor (simvastatin) went generic?
There are no insulins on the list, so I wonder if there other absences.
What does it say about the U.S. that 3 of the top 6 indications for therapy are pain, depression and anxiety?
Wednesday, October 14, 2009
Geriatric nephrology hits the NEJM
The second article in this week's Journal is Functional Status of Elderly Adults before and after Initiation of Dialysis.
The introduction references the following study and states that in 1999:
- Nursing home residents represented 4% of the people starting dialysis
- Nursing home residents represented 11% of the people initiating dialysis over the age of 70
- First year mortality is 35% for patients older than 70
- First year mortality is 50% for patients older than 78
The investigator used the USRDS and The Minimum Data Set, a database of nursing home residents that all Medicare and Medicaid certified nursing homes must participate contribute to. The study cohort consisted of people who were in the nursing home prior to starting dialysis. Patients were included if they had a functional status assessment prior to initiating dialysis. This resulted in a cohort of 3,702 residents.
Functional status was measured by grading the following skills on a scale from 0 (total independence) to 4 (dependence):
- eating
- dressing
- toileting
- maintaining personal hygiene
- walking
- getting up out of a chair
- moving around in bed
Increases in scores A second measure of functional status, MDS-ADL, was also used. Demographic, co-morbidity data was collected from the Form 2728 genereated by the nephrologist at the time of the initiation of dialysis.
200 patients were excluded from the analysis because they failed to have a funcrional status assessment prior to starting dialysis. These patients were healthier than the study cohort. I don't feel this is a critical bias as this represented a rather small fraction of the cohort. My guess is the results of this study fairly represent the population of dialysis nursing home residents.

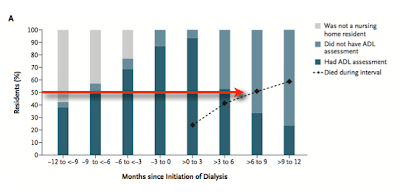
The key points are beautifully rendered in two charts. The first shows the mortality of the cohort following the initiation of dialysis:
The bars represent the timing of the ADL assessment. The dotted line is cummulative mortality. The red arrow is the half-life of this population. Half the cohort is dead before 9months!
Looking at the mortality alone one must wonder if the patients are receiving any survival benefit from dialysis. It is hard to imagine the mortality is much worse if they didn't get dialyzed.
The meat of the article is in next graph that shows the distribution of functional status every 3 months. It goes back a year prior to initiating dialysis and follows forward for the first year after initiating dialysis. Patients demonstrate a stable functional status until the 3 months prior to starting dialysis. In the three months prior to initiation there is some subtle decreases in functional status but that really accelerates as soon as they start dialysis.
The combined end points of death and deterioration are shown in a bleak graph:

What a depressing study, both mortality and morbidity. It forces nephrologists to question the role of dialysis in nursing home residents. This is a population that does terrible on dialysis.
Tuesday, October 13, 2009
After 20 years of learning I still get clinical scenarios that are total blanks

I have a patient who had an Type B aortic dissection from her left subclavian artery to somewhere south of the renal arteries. She was managed medically. Today, a decade removed from the aortic dissection, she was admitted with recurrent expressive aphasia. As part of that work-up she received a carotid doppler that did not show carotid narrowing as we were looking for but rather a carotid tumor.
She received a CT angiogram of her neck to evaluate the tumor. The CT scan revealed bilateral upper lobe pulmonary emboli. As far as we can assess these have been asymptomatic. I told her we are going to anticoagulate her but and she refused on the basis that it could worsen her dissection. The dissection was still present on the most recent CT scan.
What a bazaar scenario:
- Decade old type B aortic dissection
- recurrent TIAs
- carotid bulb tumor
- bilateral pulmonary embolism
- patient belief that anticoagulation is bad for patients.
Here is a review of conservative aortic dissection management from the Annals of Thoracic Surgery.
We examined all case records for acute (less than 2 weeks) type B aortic dissection treated at The Mount Sinai Hospital since 1985. The review identified 68 patients, 42 male and 26 female, with ages ranging from 32 to 96 years (mean, 65.5 years)...
... Follow-up ranges from 0 to 112 months (mean, 31 months). Medical therapy consisted of aggressive antihypertensive and ``antiimpulse'' therapy. Patients with unremitting pain or uncontrollable hypertensiondespite this regimen underwent early operation. Urgent operation was also performed for rupture or significant aortic dilatation (greater than 5 cm). Recently, malperfusion, initially an indication for operation, has been relieved using percutaneous catheter fenestration [1–3]...

No difference was found in one or five year survival when the cohort was divivded by the timing of the surgery. No attempt was made to look at the year of enrollment and whether that a difference in survival.
Another case series: Management and long-term outcome of aortic dissection. (Full Text). Mixes Type A and B patients.
Wednesday, October 7, 2009
Proteinuria in pregnancy

I stumbled across a good online resource for evaluating proteinuria in pregnancy. This review article is detailed and fully referenced.
Saturday, October 3, 2009
Pharma and Medical Education

Jose Arruda, Chief of Nephrology, UIC Medical Center
I was excited to see Dr. Arruda on the schedule to speak at our fellowship. This is one of the best aspects of being an academic nephrologist; we get prominent nephrologists from around the country to speak to our department.
When I saw the title of his lecture was A New Approach to Hyponatremia, I knew we were going to get the vaptan story (PDF).
Otsuka is pushing tolvaptan (Scamsca™) hard. We are getting detailed a lot, and I hear that the cardiologists are also getting an earful. Honestly, the data looks a little thin to me. The drug is the most reliable method for tackling persistent SIADH. But that's rare. In my experience, usual care fixes almost every case of hyponatremia within a day or two. There are a minority of cases that don't respond quickly. These episodes of persistent hyponatremia worry me. Unfortunately, tolvaptan doesn't feel like a good option for these patients. We know from the SALT studies that a week after you stop the drug the sodium equals the control group and the drug costs $300 per day (average wholesale price (PDF), retail price). I find it hard to prescribe a $9,000 per month drug for chronic therapy. I'll stick with salt tablets, furosemide and water restriction.

Arruda's lecture was on tolvaptan and the first slide was giving some background on hyponatremia and he commented that "I hate this slide." I can't imagine putting together a presentation and flying 500 miles to present it and loathing the very first slide.
It is illustrative of what is wrong with academic nephrology. Dr. Arruda hates the first slide in his deck. Why doesn't he remove/fix/change the slide? Because the slide deck has been vetted by the FDA and Otsuka's lawyers. He can't change it. He has signed a contract saying he won't change it. Dr. Arruda gave a solid, thoughtful lecture to our department, but he did that in spite of the materials he was using. He spent considerable time just talking about the pathophysiology of sodium and did a better job than most at avoiding being a mere shill for Otsuka.
Our nephrology program, and I suspect others (most?) rely on the generosity of pharma companies to bring scientists to our program but we pay by letting the drug companies supply the slides. Tragically, those slides are vetted by people uninterested in education and devoted to meeting the conflicting demands of both the marketing and legal departments.
Dr. Arruda seems like a good guy and is a highly respected nephrologist but the only way we could get him to come to Detroit was on Otsuka's dime and they were able to control the message.
Thursday, October 1, 2009
Highest PTH
Intact PTH of 3,420.7 in a dialysis patient. Calcium 9.7 phos 6.1. On 18 mcg of paricalcitol q treatment and cinacalcet 90 mg daily. Patient is getting excellent dialysis with eKt/V of 1.69 on 210 minutes of dialysis.
Subscribe to:
Posts (Atom)