In a previous
entry I reviewed the iPhone app
PubMedOnTap. I used this application to find articles regarding the question of whether iodinated radiocontrast media harms residual renal function for patients on dialysis. I came up with two "hits."
The Palevski study is a retrospective analysis of PD patients with residual renal function who underwent coronary angiograms. They compared residual renal function after the angiogram to previous residual renal function. They also looked at mortality, change of modality and peritonitis. They created a control group composed of patients matched for time of initiation of PD, age, and diabetic status.
29 patients met the enrollment criteria. Residual renal function was assessed an average of 14.7 weeks following the procedure. 1 patient became permanently anuric following the angiogram.
The average loss of renal function for the cases was 0.09 ml/min/month versus 0.07 ml/min/month for the controls (p=0.53). Average decline in residual renal function for PD patients is said to be 0.1 mL/min/month.
5 patients had no residual renal function measured after the angiogram and a medical record review could not document why this happened. They were censored from the final analysis.
The Janousek study is a more rigorous design, as it is controlled. They did a matched cohort study of hemodialysis patients who underwent a endovascular procedures and matched them to similar patients who did not receive contrast.
All the participants had to have at least 500 mL of urine production per day.
The contrast patients received an average of 99 mL of iodixanol (isoosmolar contrast, Visipaque) with a range of 60-180 mL.
The authors specifically state that
Our aim was not to evaluate the immediate effect of contrast medium on residual renal function during the several days after application. Rather, we wanted to evaluate its long-term clinical effect. This is why we compared the volume of daily diuresis and RREC 3 months before and 3 months after ICA administration.
They found no difference in the rate of loss of residual renal function whether they measured it by urine volume (p=0.855) or creatinine clearance (p=0.573).
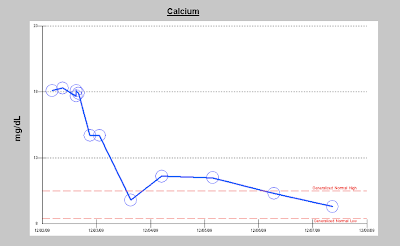
From the change in urine volume (the top chart), the value of a placebo group becomes clear. The contrast group does lose urine volume, but they lose it at roughly the same rate as the control group.
One of my concerns about the study is that since it was retrospective they purposefully restricted their analysis to patients who survived for the entire 6 month follow up period. From the Materials and Methods section:
Only clinically stable patients with no serious concomitant disease and who survived for a 6- month follow-up period with an unchanged dialysis strategy were evaluated.
So if contrast caused pre-mature death in dialysis patients, subjects having that outcome would not have been studied.
In the discussion the authors mention three other articles on the same subject:
They found two in NDT in addition to the pavlesky article. None showed a deleterious long term effect of contrast.
- The first was a prospective trial by Dittrich el at. of 10 peritoneal dialysis patients with 8 patients as controls. They found a temporary drop in residual renal function that was erased after 30 days.
- The second was a prospective cohort trial by Morrane et al. of 72 peritoneal dialysis patients, half of which were exposed to contrast. After two weeks there was no difference between the two groups or from baseline figures in regards to CrCl, urine volume or residual renal function.


















 :
: