What is wrong with this picture?
Sevelamer and Fleet Enema. They go together like a honey baked ham and Chanukah. Fleets enemas have an obscene amount of phosphorous and sevelamer (Renvela) is a phosphorous binder.
They should never co-mingle on the same MAR. So while some may see a couple of benign medications, I see a Chanukah ham.
A Fleets enema, or any typical sodium phosphorous enema, is roughly 4 onces or 120 ml. The active ingredient is sodium phosphorous, to the tune of 26g of sodium phosphate per dose, some articles quote a phosphorous concentration of 13,000 mg/dL. Remember, a normal diet has about 1 gram of phosphate and only 700 mg of that is actually is absorbed; so we are talking about a potentially massive overdose.
 |
| I love that someone scanned the entire packaging |
No patient with kidney disease or on dialysis should get this drug without talking to their doctor.
Its written right on the damn package.
I guess, if you are in the hospital and the doctor orders it, that is essentially the same thing as asking your doctor. Too bad that over and over again doctors express their ignorance about dangerous this seemingly innocuous medication can be by ordering it in patients with kidney disease.
 |
| A rogues gallery of bad outcomes from the lowly Fleets Enema |
The sodium phosphorous enema can be lethal to a patient with kidney failure.
Here is a
case report regarding a patient who developed hypocalcemic tetany and coma following a single enema
My favorite quote in the case report is the
hyperphosphatemia review of systems:
...the family denied that other drugs or unusual food such as star fruit was given by them- selves.
They gave the patient a couple of amps of calcium gluconate and then dialyzed him on hospital day 6, 7 and 8.
The situation is even more harrowing if you
give the enema orally. This results in massive sodium and phosphorous absorption. In
this case report the team gave it to the patient...twice:
They ran in to trouble while treating a toxic theophylline level. They gave activated charcoal to bind the theophylline. Subsequently, the patient developed an illeus and was given 120 mL of a sodium-phosphorous enema down the NG tube. The next day he received 4 liters of polyethylene glycol via the NG and finally another 120 ml sodium phosphorous enema enterally.
Then he arrested.
They resuscitated him. Here are his post-code labs:
- Na 177
- K 2.8
- CO2 18
- Cr 3.4
- phosphate 59.6
- calcium 5.2
- Ca x Phos product: TFTC*
- pH 7.12/37/40
* Too frightening to calculate
After resuscitation the patient was too hemodynamically unstable for dialysis and died during a subsequent arrest.
Look at that phosphorous! A phosphorous over fifty is like a traffic accident, can't tear your eyes away.
Here's a simple rule:
If the medicine is supposed to go in the butt, don't feed it to your patient.
As high as the phosphorous is however, the symptoms are due to the low calcium. The high phosphorous complexes with the calcium driving the ionized calcium down.
JASN published a tight review in 1996. They discuss an unfortunate case where a gentleman was prescribed two enemas for a flexible sigmoidoscopy prep. The patient however, mistakenly ingested them orally rather than, you know, using them the right way. 191 mmol of sodium and 208 mmol of phosphorous down the hatch. The patient presented to the ER complaining of foot and hand pain along with diarrhea and difficulty swallowing and speaking. Data on presentation:
- QTc 0.6 sec (prolonged)
- ionized calcium 0.34 mmol/L
- total calcium 4.5 mg/dL
- Na 154 mmol/L
- phosphate 44.8 mg/dl
- anion gap 39
The patient was managed with insulin and dextrose, aluminum hydroxide and IV calcium gluconate along with IV fluids. Dialysis was delayed for 4 hours due to difficulty gaining IV access. He was dialyzed against a high (3.5 mg/dl) calcium bath
One of the points I tried to highlight in the graph is the rapid drop in the phosphorous prior to the dialysis. The conservative therapy of IV fluids, insulin, and aluminum hydroxide look highly effective. Also note how effective dialysis is at raising the calcium.
The authors make an excellent point regarding the acidosis. The patient had an initial pH of 7.28 and an anion gap of 39. The anion gap is from the high phosphorous. The authors point out that treating the acidosis with alkali will further drop the ionized calcium and is contraindicated until the calcium is corrected.
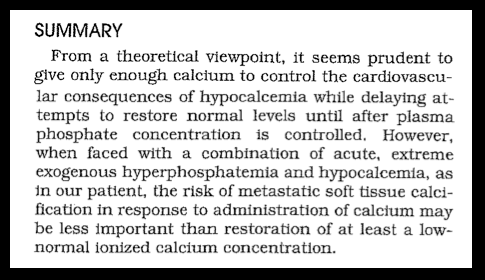
The discussion of the paper is delicious and addresses a situation I have found myself debating with fellows. The question is what to do when the phosphorous is really high and the patient has hypocalcemic symptoms. Does the administration of calcium lead to metastatic calcification to the detriment of the patient? The authors feel that calcium should be given to treat the symptoms of hypocalcemia and delay full treatment of hypocalcemia until the phosphorous is restored to normal levels.
In terms of personal experience, the MAR from the top of the post comes from a dialysis patient who did receive a Fleets enema while in the hospital. His phosphorous went from 3.5 to 11.7, overnight. He remained asymptomatic but the whole experience terrified me.
No. No. No Never. Give a fleets enema to a dialysis patient.